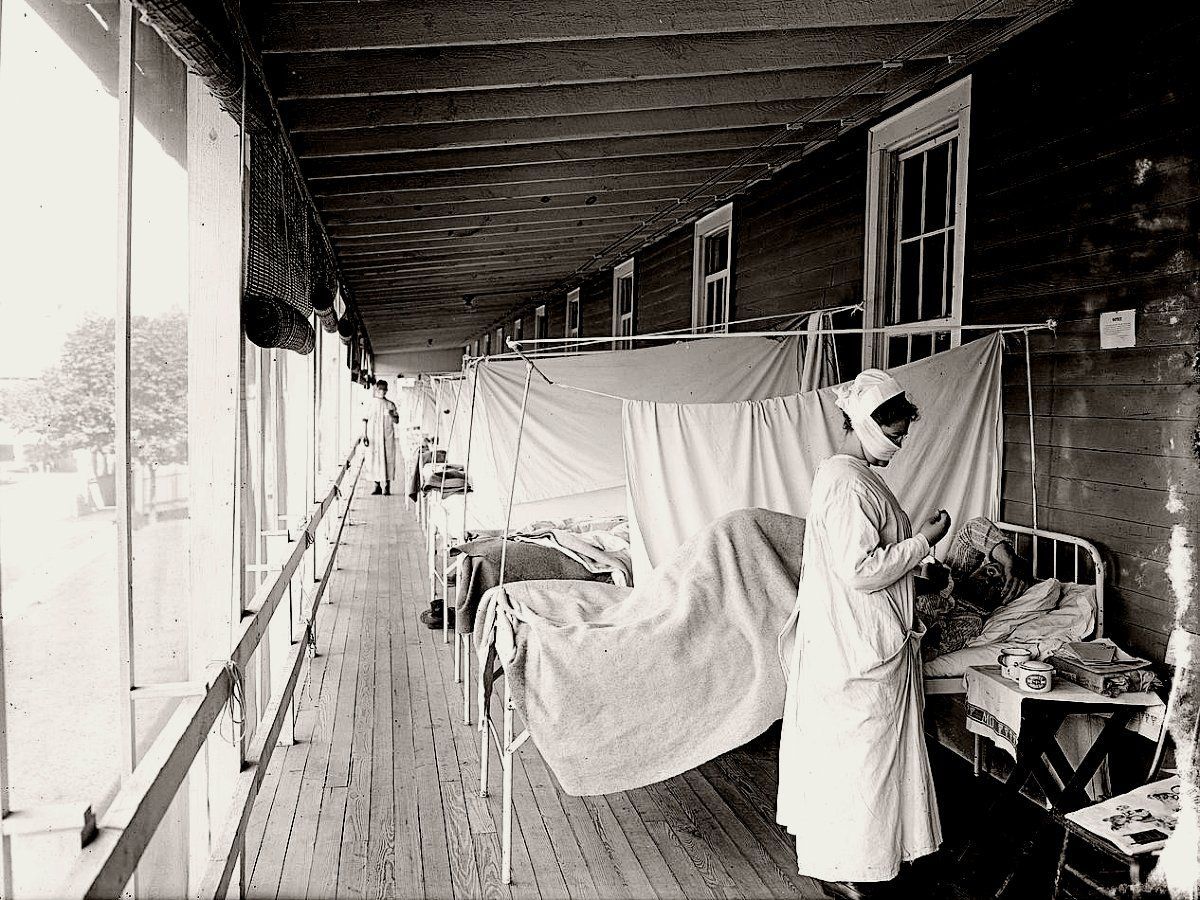
Humans have a long history of suffering infectious diseases outbreaks. A century ago, the 1918 Spanish Flu killed at least 50 million people due to a particularly high mortality rate. Similarly severe outbreaks occurred again in 1956 and 1968, killing a further three million people across two different flu pandemics.
Prior to modern times, the recurrence of the bubonic plague killed hundreds of millions of people, wiping out a significant percentage of regional populations wherever it struck. Throughout human history, Malaria is thought to have potentially killed nearly half of all humans who have ever lived, and still kills at least half a million people each year.
While advancements in medical technology have allowed us to better manage outbreaks over the past several decades, this trend may not be able to continue forever. With more humans and farm animals alive now than ever before, more people than ever before living in densely packed urban areas with poor sanitation, the rise of chronic illness and antimicrobial resistance, and the future threat of climate change, our risk of experiencing a major global pandemic may be increasing.
Here's an overview of some of the current risks we face when it comes to infectious disease outbreaks.
1. Unsustainable Animal Agriculture
Factory farms are breeding grounds for all kinds of nasty pathogens. Worldwide, tens of billions of land animals are killed each year for human consumption. In most cases, their brief lives are spent suffering in the confines of their cramped enclosures, unable to freely move around and in some cases never seeing the light of day.
This has all of the ingredients for an epidemic outbreak to occur. Animals raised for their meat are typically given low-quality and pesticide-laden food, stuffed full of antimicrobial medicines to both ward off disease and encourage growth, kept in unsanitary conditions, and exposed to environmental toxins that can destroy their immune systems [1]. All of these factors add up to animal agriculture being the single biggest risk for causing a global pandemic.
It's no secret that animal agriculture presents a huge risk of a global outbreak occurring. From chicken and other poultry, avian flu has been a huge concern for decades, with DNA analysis suggesting that the Spanish Flu of 1918 arose from an avian flu strain. From pigs, swine flu and the recent outbreaks of African swine fever—which kills almost any animal it infects—represent a relatively new risk. It's now expected that nearly half of China's pig herd (by far the largest in the world) will have been culled and destroyed by the end of 2019 as a result of the disease.
 Pigs confined in cramped and unsanitary conditions. Image: Wikimedia Commons.
Pigs confined in cramped and unsanitary conditions. Image: Wikimedia Commons.
Although avian and swine pathogens typically don't infect humans, the primary cause for concern is that, in some instances, they can and do mutate and become infectious to human beings. Some of the biggest influenza pandemics of the past have originated from animal influenza viruses, and it's very likely that it will happen again. It's estimated that an outbreak of a virulent animal influenza strain among the global population could end up killing anywhere from a few million to over 100 million people.
While animal influenza viruses are perhaps the most-watched pandemic risk stemming from our unsustainable animal agriculture practices, the conditions these animals live in allows for other types of pathogens—such as bacterial infections—to flourish as well.
The way the current system operates, the primary way farmers can minimize the spread of infectious diseases among factory farmed animals is with the liberal use of antibiotics. But this is creating an arms race in the animal agriculture industry, from which increasingly drug resistant pathogens are able to emerge and spread unabated. This practice is one of the key factors in the current rise of antimicrobial resistance worldwide, which is itself becoming a global health emergency.
2. Antimicrobial Resistance
Resistance to the drugs used to treat disease arises via natural evolutionary processes. Once a bacterium evolves a resistance to a drug, it's able to quickly multiply and spread this resistant trait to other bacteria. Through this powerful natural process, the drugs normally used to treat disease gradually become ineffective.
In the animal agriculture industry, this is the arms race. Infectious bacteria are able to evolve a resistance to the antibacterial medicines we rely on to keep epidemic outbreaks among factory farms to a minimum, which then requires farmers to either increase the dosage or seek out more potent (and expensive) drugs.
As these pathogens continue to develop antimicrobial resistance, the risk is that these drug-resistant strains could then cross over to human beings and turn into an untreatable pathogen spreading among the human population.
In addition to the use of antimicrobials on factory farms, the over-prescription of antimicrobial drugs within our global health care system is a critical problem. drug-resistant super-bugs are popping up within health care facilities, with multidrug-resistant tuberculosis being just one example. As things currently stand, surgeries and medical procedures are becoming riskier, and common diseases and infections are steadily becoming untreatable and unresponsive to available medications.
The repercussions of our overuse of antibiotics are severe. The United Nations has warned that if no action is taken, drug-resistant diseases could cause 10 million deaths each year by 2050 and cause catastrophic economic damage—this up from the estimated 700,000 people who currently die each year as a result of drug resistant strains. This has led some experts in global health to classify this increasing drug resistance as a pandemic of its own.
To make matters worse, these chemicals are entering our natural environment through wastewater and discarded trash (similarly to microplastics). Once there, these drugs wreak havoc on our ecosystems and the organisms that live there, further increasing the risk of environmental pathogens developing a resistance to antibiotic and antifungal medicines.
The over-use of antimicrobial medicines doesn't just increase risk by pressuring pathogens to develop drug resistance, it also has a tremendously bad impact on human health in general. These chemicals don't just target the bad bacteria—they also target the good bacteria that constitutes our microbiome, a key component of our body's natural immune system [2].
Compromising our body's natural microbiome through exposure to antimicrobial chemicals ends up making us more susceptible to both pathogens and chronic disease down the road, and not having this natural defense against bad bacteria makes new infections more likely and riskier. This becomes a catch-22: our increasing susceptibility to infections and their increasing resistance to drugs causes health professionals to prescribe increasingly potent antimicrobials in order to manage illnesses. In turn, pathogens exposed to more potent drugs are able to develop resistance to those chemicals as well.
 An Ebola isolation ward prepared to accept patients. Image: CDC Global / Bryan Christensen.
An Ebola isolation ward prepared to accept patients. Image: CDC Global / Bryan Christensen.
Studies of the animals agriculture industry have also shown that our food is susceptible to contamination in the form of antimicrobial residues found in meat. Extensive use of these chemicals in animal agriculture may cause humans to develop drug resistance, suffer reactions to drug exposure, experience intestinal flora disruption, and prolonged exposure could lead to the development of cancers, chemically-induced DNA disruption, or impede the normal development of human embryos [3].
With the presence of antimicrobial chemicals in our food supply, in our environment, and in in our health care system, it's no wonder an increasing number of once treatable bacteria are developing a resistance to the drugs we've been relying on for decades.
This all adds up to an increased risk that the next global pandemic will arise from a pathogen that has a built-in resistance to our available medicines, rendering the infection untreatable. On top of that, the ever-present antimicrobials we're continually exposed to may be playing an large role in the global uptake in chronic illnesses.
3. The Rise of Chronic Disease
Not only do we need to contend with the fact that some of the nastiest pathogens arise from animal agriculture, and that an increasing number of these pathogens are developing resistance to our drugs—we also need to acknowledge the fact that an increasing portion of the global population is starting off from a point of un-health.
In the United States, for example, nearly half of people aged 65 and over have at least one chronic health condition that puts them at increased risk for experiencing complications related to influenza. Further, nearly 10% of the population of the United States has diabetes, which puts people at a 6x risk of hospitalization due to influenza, and 3x higher risk of death.
With exposure to antimicrobials and a plethora of other factors resulting in compromised immune systems and contributing to the rise of chronic disease, a global pandemic could put incredible strain on our relatively ill-prepared health care system. With more people needing to be hospitalized than the number of beds available, and the probability that antibiotic resistance could hamper effective treatment, it's very possible that any sufficiently infectious pathogen could overwhelm our ability to manage it and result in a large spike in mortality as a result [4].
The risk of an infectious disease aside, the unprecedented rise in chronic disease has itself been labelled as a global pandemic [5]. This combination—an immune-compromised population, a highly infectious and virulent strain that has also developed resistance to most conventional antibiotics—has the potential to cause devastation on a scale similar to that of the Spanish Flu of 1918.
4. Urbanization and Globalization
As our world becomes more populated, it's also becoming more urbanized—and urbanization doesn't always take the form of skyscrapers and expensive infrastructure projects.
As more and more people across the developed and developing world move into cities, in many cases, infrastructure improvements can't keep up. When it comes to pandemic risk, overcrowding and poor waste management in cities across the developing world is of particular concern [6].
In addition to contaminated water sources and the lackluster waste management, these poorer communities in which outbreaks are more likely to occur are also the least likely to have access to adequate medical treatment.
 A pop-up Ebola isolation center in Sierra Leone in 2014. Image: CDC Global.
A pop-up Ebola isolation center in Sierra Leone in 2014. Image: CDC Global.
Above and beyond poor infrastructure making outbreaks more likely to occur, other human factors such as population density, air travel, and global trade all have a sizable impact on the ability for a local epidemic to quickly spread and become a global pandemic.
The way we utilize land in order to sustain our urban centers can also have a detrimental impact: the proliferation of animal agriculture, industrial development, and natural resource extraction all create additional stress on the local ecosystem. Not only are our cities overpopulated, they're also surrounded by an environment that's tainted by synthetic chemicals, heavy metal contamination, microplastics, and waste/pesticides from animal and plant agriculture—any of which may be concentrated in our air, water, and/or soil.
When it comes to pandemic risk, an unhealthy and unbalanced ecosystem that experiences a loss of biodiversity is also more likely to produce infectious pathogens [7].
5. Pandemic Outbreaks in Conflict Areas
As we're seeing now with the ongoing Ebola outbreak in the Democratic Republic of the Congo (DRC), the threat of violence from numerous armed groups and militias makes treating infectious diseases significantly more challenging.
The World Health Organization recently declared a Public Health Emergency as a result of the ongoing Ebola crisis, largely as a result of the challenges doctors and aid workers have been facing amidst the ongoing armed conflicts in the regions affected by the latest Ebola outbreak.
While Ebola in its present form is unlikely to escalate into a full-scale global pandemic, there's always a risk that it could mutate to become more infectious or difficult to contain (ie. if the experimental vaccine stops having an effect). The presence of armed conflicts in an active outbreak zone makes containment significantly more difficult [8].
In addition to preventing effective treatment on the ground, armed conflict also leads to refugees dispersing into surrounding areas. Several new cases of Ebola have now been confirmed in towns bordering other African nations, and the risk here is that refugees fleeing conflict zones will transmit the disease to other regions.
But it's not just migrating refugees that's a cause for concern: ongoing conflicts also destroy livelihoods and infrastructure, which creates the conditions for pathogens to emerge.
An example of this has been seen in Yemen over the past few years. Over one million cases of cholera have been reported amidst the ongoing civil war and aerial bombardment by Saudi Arabia, which have caused massive damage to the country's infrastructure. With sanitation severely compromised and untreated wastewater free to leak into drinking water sources, an outbreak of cholera was almost inevitable.
A similar situation is now unfolding in the DRC, where a vaccine campaign is being deployed to protect against a Measles epidemic in addition to the ongoing Ebola crisis.
To complicate matters further, thousands of people have fled their homes and are now living in displacement camps where the threat of cholera and malaria are also exacerbated by unsanitary conditions. There's truly no better example of Hell on Earth when it comes to conflict-driven epidemics than what's happening in the DRC in 2019.
6. Climate Change
If it weren't enough that global pandemic risk is driven by the food we eat, the medicines we use, the environments we live in, and the global security issues we face, we also need to recognize the future impact a changing climate will have on emerging diseases.
It's a known fact that in hotter and more tropical climates, more viruses and bacteria are able to thrive. This is why, in general, regions nearer to the equator have an outsized infectious disease burden when compared to regions nearer to the poles. The science has shown that, as a result of a warming climate, Lyme-disease carrying ticks are now able to survive in regions that were previously too cold for them.
As the Earth warms due to anthropic emissions of greenhouse gasses, more and more diseases are going to be able to survive in environments that they were previously unable to live in. It's not a question of whether or not a changing climate will increase the number of epidemics we face—but rather how severe this effect will be.
A study which modeled the current and future threat of Dengue fever found that the range of the Dengue virus could extend further into North America and encompass a much greater area of Africa as the climate continues to warm, putting greater numbers of humans at risk of contracting the mosquito-borne virus.
As with other factors increasing the risk of a global pandemic, climate change doesn't just create risk by expanding the territory in which any given pathogen can spread. A changing climate also brings more extreme weather events—hurricanes, floods, droughts, and unpredictable weather patterns that can enable outbreaks to occur more frequently. But perhaps the biggest wild card when it comes to pandemics and climate change is that it's difficult to quantify exactly what the end result might be.
Sources & Further Reading:
[1] Winans et al, 2010. "Environmental toxicants and the developing immune system: a missing link in the global battle against infectious disease?"
[2] Shi et al, 2017. "Interaction between the gut microbiome and mucosal immune system"
[3] Okocha et al, 2018. "Food safety impacts of antimicrobial use and their residues in aquaculture"
[4] Madhav et al, 2017. "Disease Control Priorities: Improving Health and Reducing Poverty. 3rd edition"
[5] Terzic, Andre, and Waldman, Scott, 2011. "Chronic Diseases: The Emerging Pandemic"
[6] Neiderud, Carl-Johan, 2015. "How urbanization affects the epidemiology of emerging infectious diseases"
[7] Ostfeld, RS, 2009. "Biodiversity loss and the rise of zoonotic pathogens"
[8] Gayer et al, 2007. "Conflict and Emerging Infectious Diseases"